Plantar
Fasciitis
Plantar Fasciitis (or fasciopathy) is a condition of pain and tissue damage at the attachment of the plantar fascia to the underside of the calcaneus (heel bone).
Anatomy
The plantar fascia is a band of connective tissue that runs along the sole from the heel to the ball of the foot. One of its main roles is to keep the bones and joints in position and enables us to push off from the ground. Bruising or overstretching this ligament can cause inflammation and heel pain. In many cases, plantar fasciitis is associated with a heel spur. Surprisingly, the spur itself does not cause pain, and may often be found in the other foot without symptoms.
Risk
- Certain sports – Activities that place a lot of stress on the heel bone and attached tissue, i.e., running, dance and aerobics.
- Flat-footed or high arches – People with flat feet may have reduced shock absorption, increasing strain on the plantar fascia. High arched feet have tighter plantar tissue, leading to similar effects.
- Middle-aged or older – Heel pain tends to be more common with ageing as muscles supporting the arch of the foot become weaker, putting stress on the plantar fascia.
- Overweight – Weight places a greater mechanical load on the plantar fascia. There is evidence that overweight and inactivity lead to chemical damage to the plantar fascia, with a worsening of pain.
- Pregnancy – Weight gain, swelling and hormonal changes that accompany pregnancy may lead to mechanical overload of the plantar fascia.
- Being on your feet – People with occupations that require a lot of walking or standing on hard surfaces may suffer plantar fascia pain.
- Wearing shoes with poor arch support or stiff soles – Poorly designed shoes may contribute to problems.
Prevention
- Maintaining a healthy weight to minimise the stress on the plantar fascia.
- Choosing supportive shoes. Avoiding stiletto heels and shoes with excessively low heels. Buying shoes with a low to moderate heel, good arch support and absorption. Not going barefoot, especially on hard surfaces.
- Not wearing worn-out runners. Replacing old runners before they stop supporting and cushioning the feet. If a sport involves a lot of running, replacing shoes after about 650 kilometres of use.
- Starting activity slowly. Warming up before starting any activity or sport, and starting a new exercise program slowly.
- Undertaking training prior to competition to ensure readiness to play.
- Allowing adequate recovery time between workouts or training sessions.
- Checking the sporting environment for hazards.
- Drinking water before, during and after play.
- Avoiding activities that cause pain.
Signs and Symptoms
Pain is usually felt on the underside of the heel, and is often most intense with the first steps of the day or after rest. It is commonly associated with long periods of weight bearing or sudden changes in weight bearing or activity.
You may experience:
- Sharp pain in the inside part of the bottom of the heel, which may feel like a knife sticking into the bottom of the foot.
- Heel pain that tends to be worse with the first few steps after awakening, when climbing stairs or when standing on tiptoe.
- Heel pain after long periods of standing or after getting up from a seated position.
- Heel pain after, but not usually during, exercise.
- Mild swelling in the heel.
Immediate Management
Initial treatment includes gentle stretching of the Achilles tendon and plantar fascia, weight loss, taping, arch support and heel lifts. Difficult cases may be referred for physiotherapy. Physiotherapy includes myofascial release and scar tissue breakdown of the plantar fascia, and supervised stretching. A strengthening program for the calf muscles and small muscles of the foot is important. Be aware that this may increase soreness initially, but persistence should be rewarding.
Care should be taken to wear supportive and stable shoes. Patients should avoid open-back shoes, sandals, ‘flip-flops’, and any shoes without raised heels. A podiatrist can assist with plantar fasciitis and other foot and lower limb problems.
Treatment
For most people, the condition improves spontaneously within a year. Treatments that may help control symptoms include:
- Night splints – A sports medicine professional may recommend wearing a splint fitted to the calf and foot while sleeping. This holds the plantar fascia and Achilles tendon in a lengthened position overnight.
- Orthotics – A sports medicine professional may prescribe off-the-shelf or custom-fitted arch supports (orthotics) to help distribute pressure to the feet more evenly, and to stimulate the small foot muscles.
- Physiotherapy – A physiotherapist can give instructions on a series of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles, which stabilises the ankle and heel. A physiotherapist may also instruct how to apply athletic taping to support the bottom of the foot.
- Medication, injection and surgery – These measures are for the most persistent cases, and do not replace the need for the treatment methods detailed above.
Rehabilitation and Return to Play
Aims of rehabilitation
- Decrease initial pain and inflammation.
- Identify biomechanical dysfunction.
- Improve flexibility.
- Strengthen the plantar fascia.
- Return to full fitness.
- Injury prevention.
Reducing pain and inflammation
- Reduce activities that cause pain.
- Maintain fitness by swimming or cycling. Take the opportunity to work on upper body strength.
- Taping gives excellent support while allowing the foot to heal.
- If taping is effective then it is likely that orthotics will also be effective in correcting foot biomechanics and helping to prevent the injury returning once normal training has resumed.
- Apply cold therapy. Ice massage for 10 minutes to the site of pain – several times a day if possible. A frozen drink bottle used like a rolling pin is an easy way of performing ice massage.
Return to play
- Follow the advice given by a sports medicine professional.
- After a week of no pain running can be started again.
- This should be a gradual process. If pain is felt at any time then go back a step.
- Running time should be gradually increased.
- Apply tape to the foot to support it for the first few runs, especially if orthotics are not being worn.
- Ensure the correct shoes for your type of running style or sport are worn.
- After every training session apply ice for about 10 minutes.
- Stretch properly before each training session and after. Hold stretches for about 30 seconds and repeat five times.
Acknowledgements
Sports Medicine Australia wishes to thank the sports medicine practitioners and SMA state branches who provided expert feedback in the development of this fact sheet.
Images are courtesy of www.istockphoto.com
Always Consult a Trained Professional
The information above is general in nature and is only intended to provide a summary of the subject matter covered. It is not a substitute for medical advice and you should always consult a trained professional practising in the area of sports medicine in relation to any injury. You use or rely on the information above at your own risk and no party involved in the production of this resource accepts any responsibility for the information contained within it or your use of that information.
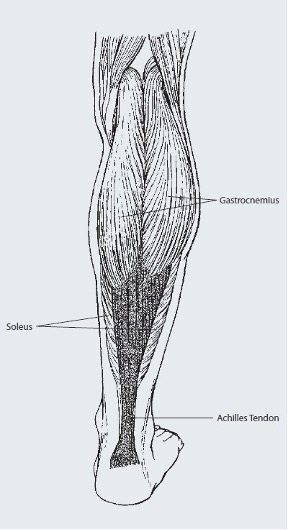
The Achilles tendon is a large tendon at the back of the ankle. The tendon is an extension of the gastrocnemius and soleus (calf muscles), running down the back of the lower leg attaching to the calcaneus (heel bone). The Achilles tendon connects the leg muscles to the foot and gives the ability to push off during walking and running.
Risk
The two most common injuries of the Achilles tendon are Achilles Tendinopathy, and tearing or rupturing of the tendon. Other less common injuries include Peritendinitis and Retrocalcaneal Bursitis. Achilles Tendinopathy can be due to one or a number of causes which may result in excessive loading on the Achilles, including:
- A sudden increase in the intensity, frequency and duration of activity.
- A decrease in recovery time between activity.
- Wearing inadequate or incorrect footwear.
- Excessive pronation (force on Achilles tendon increases).
- Running on hard or uneven surfaces.
- Change of surface (seasonal).
- Poor muscle flexibility (e.g. tight calf muscles, weak calf muscles).
- Decreased joint range of motion (e.g. stiff ankle joint).
- Inadequate warm up, stretching and cool down.
An Achilles tendon rupture is a complete or partial tear that occurs when the tendon is stretched beyond its capacity. Forceful jumping or pivoting, or sudden accelerations of running can overstretch the tendon and cause a tear. An injury to the tendon can also result from falling or tripping. Achilles tendon ruptures are most often seen in ‘weekend warriors’ – typically, middle-aged people participating in sports in their spare time. Less commonly, illness or medications, such as steroids or certain antibiotics, may weaken the tendon and contribute to ruptures.
Prevention
- Wearing appropriate shoes for the activity.
- Using correct technique to limit excessive stress on the Achilles tendon.
- Strapping and taping the ankle to assist in creating a more secure structure.
- Warming up, stretching and cooling down.
- Undertaking training prior to competition to ensure readiness to play.
- Participating in regular strengthening and stretching sessions to maintain muscle strength and flexibility.
- Gradually increasing the intensity and duration of training.
- Allowing adequate recovery time between workouts or training sessions.
- Avoiding activities that cause pain. If pain does occur, discontinuing the activity immediately and commencing RICER.
Signs and Symptoms
Achilles Tendinopathy
- Mild to severe pain and tenderness in the Achilles tendon area (tenderness may be more noticeable in the morning).
- Stiffness that may diminish as the tendon warms up with use.
- Decreased strength and movement – a feeling of sluggishness in the leg.
- Achilles Tendinopathy is graded from 1-4 according to severity.
|
Grade |
Description |
|
1 (mild) |
Pain after running only |
|
2 (moderate) |
Pain before and after running; pain gradually lessons during a run. |
|
3 (severe) |
Pain with activity causing a decrease in volume of activity. |
|
4 (extreme) |
Pain during everyday activities (pain worsening or progressing) |
Achilles tendon injuries
An Achilles tendon can partially tear or completely rupture. While a partial tear presents similar symptoms as a Tendinopathy, a complete rupture causes pain and sudden loss of strength and movement. The pain is likened to a hit or kick in the back of the leg.
Immediate Management
The immediate treatment of any soft tissue injury consists of the RICER protocol – rest, ice, compression, elevation and referral. RICE protocol should be followed for 48–72 hours. The aim is to reduce the bleeding and damage within the joint.
The No HARM protocol should also be applied – no heat, no alcohol, no running or activity, and no massage. This will ensure decreased bleeding and swelling in the injured area.
Treatment includes rest, pain relief, stretching exercises, and changes in sports techniques and footwear to reduce stress on the tendon. Surgery may also be required in some instances.
Rehabilitation and Return to Play
Achilles Tendinopathy that is causing symptoms can require weeks to months of rest for the tendon to slowly repair itself. A sports medicine professional should be seen as soon as possible to determine the extent of the injury and to provide advice on treatment required.
Once pain has settled, a program of rehabilitation exercises may be prescribed to gradually strengthen the tendon to enable it to cope with increased load before return to activity.
The use of crutches may be recommended to keep weight off the injury. Taping, a heel raise or even a plaster cast may also be used if the injury is severe. Other treatments may include ultrasound, mobilisation, stretching, sports massage and orthotics. Anti-inflammatory medication may also be prescribed to reduce pain.
A completely ruptured Achilles tendon is most often repaired surgically. Surgery is often followed by immobilisation in a plaster cast for up to nine weeks. Following this immobilisation period, the Achilles tendon will require intense rehabilitation followed by a strengthening program. These will be completed under the supervision of a sports medicine professional.
Return to activity should be gradual. When returning to activity, a heel raise or taping may be used to reduce the load on the weakened Achilles tendon.
Acknowledgements
Sports Medicine Australia wishes to thank the sports medicine practitioners and SMA state branches who provided expert feedback in the development of this fact sheet.
Images are courtesy of www.istockphoto.com
Always Consult a Trained Professional
The information above is general in nature and is only intended to provide a summary of the subject matter covered. It is not a substitute for medical advice and you should always consult a trained professional practising in the area of sports medicine in relation to any injury. You use or rely on the information above at your own risk and no party involved in the production of this resource accepts any responsibility for the information contained within it or your use of that information.
